All Solutions
Explore all the solutions you can create with Paperform: surveys, quizzes, tests, payment forms, scheduling forms, and a whole lot more.
See all solutions










Connect with over 2,000 popular apps and software to improve productivity and automate workflows
See all integrationsProducts
Solutions
All Solutions
Explore all the solutions you can create with Paperform: surveys, quizzes, tests, payment forms, scheduling forms, and a whole lot more.
See all solutionsIntegrations
Connect with over 2,000 popular apps and software to improve productivity and automate workflows
See all integrationsResources
When medical procedures don't follow standard protocols—whether due to complications, multiple procedures, discontinued services, or unusual circumstances—insurance modifiers become essential for proper reimbursement. This Insurance Modifier Usage Justification Form helps medical practices document and justify modifier usage for claims requiring additional review or payment adjustments.
Built for medical billing departments, practice managers, and healthcare administrators, this template captures all the critical details insurers need to process complex claims: provider information, patient details, procedure codes with modifiers, clinical justification, and supporting documentation. Instead of scrambling through emails and spreadsheets when a claim is flagged, your team can submit a complete, professional justification that addresses payer requirements upfront.
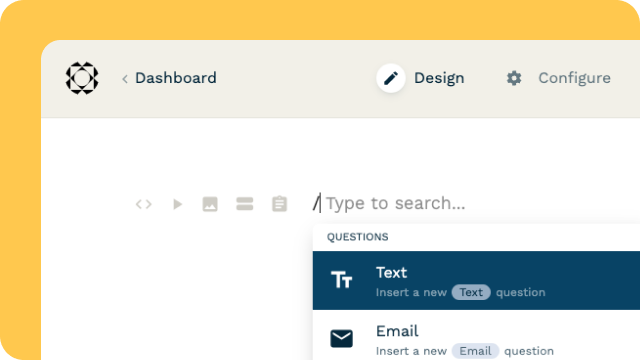
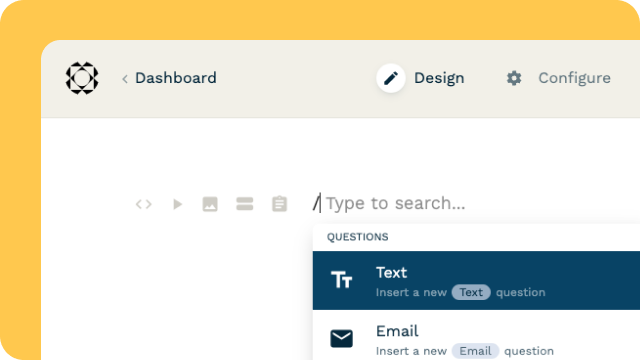
Paperform makes medical billing workflows cleaner and more compliant. Use conditional logic to show different fields based on modifier type (like detailed explanations for modifier 22 or 59), embed the form directly in your practice management portal, and connect submissions to your billing system via integrations with Google Sheets, Airtable, or your EHR through Stepper workflows. You can even set up automated email notifications to your billing team and insurance coordinators when a justification is submitted.
For practices handling high volumes of modifier-based claims, Stepper (stepper.io) can automate the follow-up process—routing submissions to the right reviewer, updating claim tracking systems, and triggering reminder workflows if payer responses are delayed. Everything stays organized, auditable, and ready for appeals if needed.
Whether you're justifying increased procedural services, bilateral procedures, staged services, or other unusual circumstances, this template gives your billing team a standardized, professional format that speeds up reimbursement and reduces claim denials.